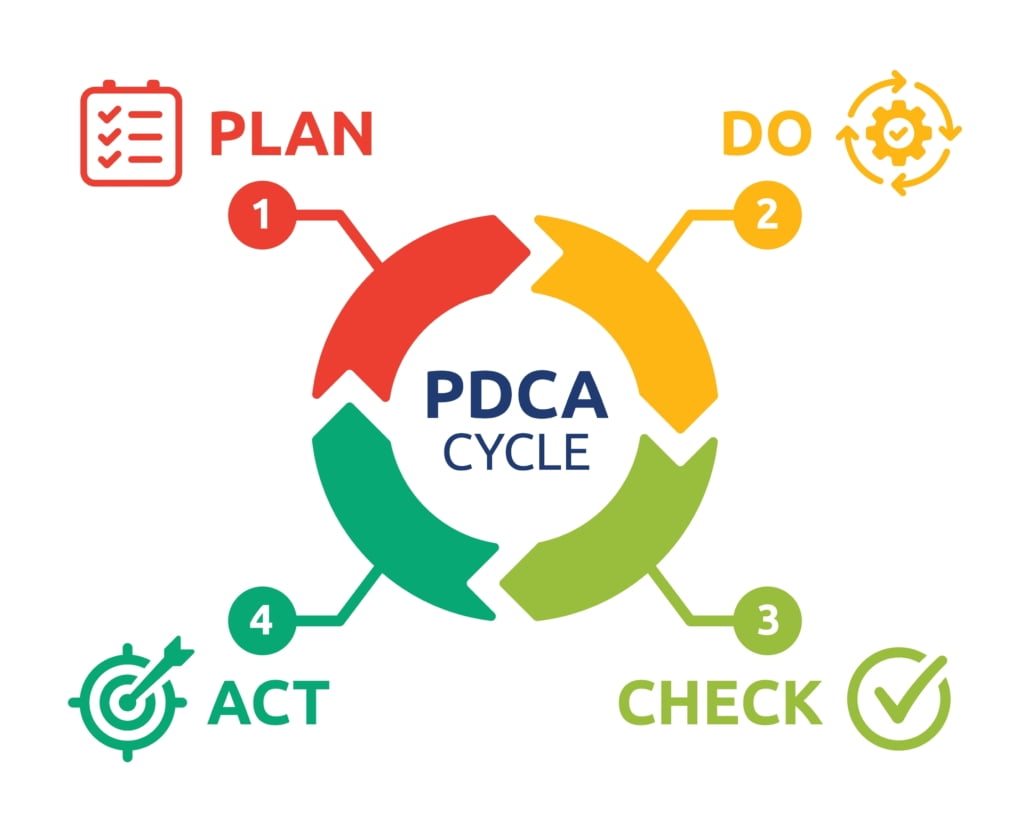
The Plan Do Check Act (PDCA) cycle: a model for continuous improvement
You’ve identified which problem or opportunity to work on, but what next? How do you make sure you spend the little time you have available to do this quality improvement in the best way possible? In this how-to guide, we’ll walk you through a systematic approach called the PDCA cycle, to guarantee you run the project like a pro!
What is It?
The PDCA cycle is a popular model used for quality improvement and change. It consists of four key phases: Plan, Do, Check, and Act, which are completed in a step-wise manner. The sequence can be repeated, promoting ongoing refinement of a solution and a culture of continuous improvement amongst the team.
Healthcare teams often add a foundation stage to the cycle in which the problem is defined and measures are established.
Why use it?
The PDCA cycle is a straightforward and versatile approach for all staff to use. It encourages the benefits of testing and learning, avoiding the extremes of over planning and rushed, ineffective changes.
How’s it used?
Step 1: Foundation
Start by identifying and defining the problem you want to solve. Find a measure that will tell you if your changes are working and baseline it. Do a root cause analysis and come up with some creative countermeasures.
Step 2: Plan
Decide on one solution to test and get everything ready to start testing it. This might involve voting on the solutions you previously identified and quickly coming up with a protocol for staff to test.
Step 3: Do
Put the chosen solution into action on a small scale. This might mean running it for a few days or with a few patients. Make sure you collect the data to indicate whether its working as you go along.
Step 4: Check
Analyse the data from the trial to determine if it’s working as expected. This might involve looking at numbers or getting feedback from staff or customers. Reflect on the results and decide whether it’s been successful, needs adjustments or you should try a different solution.
Step 5: Act
Based on what you’ve learned, take action. If the change is successful, roll it out as a new way of working. If it needs adjustments then update the protocol and validate them. If it didn’t work, prepare for the next improvement cycle.
Example
A surgical team decides it’s taking too long to get operations started every morning. They use the time between their shift starting and the induction of the first patient as the measure. They take a baseline measure of 60 minutes. They do a root-cause analysis and identify several solutions to trial.
| Cycle | Plan | Do | Check | Act |
| 1 | The team vote on changing the pre-meds they use so they’re faster acting. They agree on the new drugs and doses and select a week to pilot them. | They use a different pre-med protocol for one week and record the induction times on a post-it note by the anaesthetic machine each day. | Following the pilot they review the data. The average time is now 45 minutes. They discuss the results and decide to roll out the change. | To roll the change out they create a new pre-med chart for the wall and discuss it at their monthly vet and nurse meeting. |
Top Tips
- Set a specific timeframe to complete the cycles, like 4 weeks, in order to maintain focus on delivery.
- Involve front-line staff in the test phase as it will reduce the barriers to any final changes you roll out.
- Balance your time evenly across different areas of the cycle, avoid jumping the test or planning phase.
In summary, the PDCA cycle provides a simple and versatile model for you to use to make sure your QI project stays on track. If you need more support in getting started, or have a particularly complex problem you need help with, contact Contact VetQI



